How Long Does It Take For Platelets To Increase After Chemo
Side Effects of Cancer Treatment: Thrombocytopenia (Low Platelet Counts)
Medically reviewed by C.H. Weaver G.D. Medical Editor 8/2018
- What is Thrombocytopenia?
- Why is Chemotherapy-Induced Thrombocytopenia Important?
- How do I Know if I Have Thrombocytopenia?
- Tin Thrombocytopenia be Prevented?
- How is Chemotherapy-Induced Thrombocytopenia Treated?
- Strategies to Improve Treatment or Prevention of Chemotherapy-Induced Thrombocytopenia
What is Thrombocytopenia
Thrombocytopenia refers to the presence of abnormally depression levels of platelets in the circulating blood. Platelets, or thrombocytes, are a specific kind of blood cell that foreclose bleeding. The most common reason that cancer patients feel thrombocytopenia is as a side effect of chemotherapy. When chemotherapy affects bone marrow, the trunk's ability to produce platelets, the body's chief defence against bleeding, is diminished. Platelets normally blitz to the site of an injury and work with other blood factors to from a blood clot. Normally, there are billions of platelets in the blood; still sure chemotherapy drugs can lower the platelet count. The fewer platelets an individual has in his/her blood and the longer he/she remains without plenty of them, the more than susceptible he/she is to bleeding.
Chemotherapy-induced thrombocytopenia typically occurs 6-10 days following assistants of the chemotherapy drugs and continues for several days before platelets recover to an advisable level. Infrequently, cancer patients may besides feel thrombocytopenia from other medications or every bit a issue of their underlying cancer. When discussing the consequences and management of thrombocytopenia, it is important to distinguish between chemotherapy-induced thrombocytopenia and thrombocytopenia resulting from other causes.
The type and dose of chemotherapy also has an consequence on how depression the platelet count drops and how long it will take to recover. While receiving chemotherapy, a patient's blood may exist tested ofttimes to brand sure he/she has enough platelets. Thrombocytopenia, or "low platelets", are terms used to describe a depression platelet level in the blood. Fortunately, having a depression level of platelets can exist corrected for many patients.
Why is Chemotherapy Induced Thrombocytopenia Important
Chemotherapy involves the use of drugs to destroy cancer cells. Chemotherapy works by destroying cancer cells that grow rapidly. Unfortunately, chemotherapy as well affects normal cells that grow quickly, such as blood cells forming in the bone marrow, cells in the hair follicles or cells in the oral fissure and intestines.
When patients experience thrombocytopenia following assistants of chemotherapy, they are at risk of certain side effects. Specifically, the fewer platelets in the blood and the longer a patient remains without plenty platelets, the more susceptible he/she is to experiencing bleeding. Thrombocytopenia confers a risk of bleeding and the magnitude of hazard is closely correlated with the severity and duration of thrombocytopenia. As the platelet count falls below twenty,000-50,000; x,000-20,000; and less than 10,000 cells/µl, the frequency of life-threatening haemorrhage rises steeply from approximately 5-half-dozen% to 10% and 20-forty%, respectively. Patients developing thrombocytopenia require handling with platelet transfusions and occasionally, admission to the infirmary, until the platelets return to sufficient levels in the claret to prevent bleeding.
Thrombocytopenia is important for another reason. When patients are treated with chemotherapy, it is for the purpose of destroying cancer cells in order to reduce symptoms from their cancer, prolong their survival or increment their adventure of cure. Chemotherapy may exist administered every bit a single drug or in combination with several drugs. The combination of chemotherapy drugs administered to a patient is referred to as a treatment regimen. In a chemotherapy treatment regimen, drugs are administered to patients at a defined dose and according to a specific time schedule. The dose and time schedule of drugs administered in the chemotherapy regimen has been scientifically derived to produce the best chance of survival or cure. When patients develop thrombocytopenia following administration of chemotherapy, doctors may take to delay treatment or reduce the doses of the chemotherapy. Clinical studies have shown for certain diseases that when the dose of therapy is reduced or the handling cycles prolonged, patients have lower cure rates than if they had been able to receive therapy at the full dose on schedule. Fortunately, there are strategies for the treatment of chemotherapy-induced thrombocytopenia that accept been proven to reduce the need for platelet transfusions and help patients receive their treatment on schedule.
How Exercise I Know if I Have Thrombocytopenia
A consummate blood count (CBC) measures the levels of the 3 bones blood cells: white cells, red cells and platelets. In the United states of america, the CBC is typically reported in the following format:
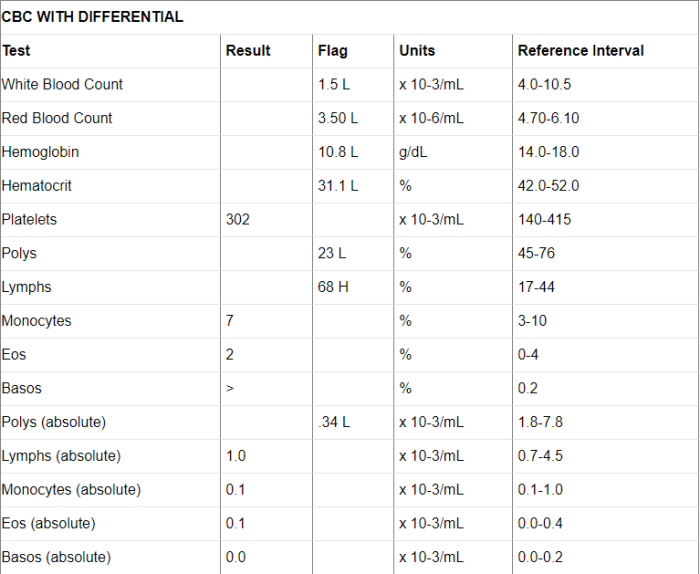
Consequence column: The result column shows counts that fall inside the normal range.
Flag cavalcade: The flag column shows counts that are lower ("L") or higher ("H") than the normal range.
Reference Interval (or Reference Range) column: The reference interval shows the normal range for each measurement for the lab performing the test. Different labs may use different reference intervals.
White blood cells: White blood cells help protect individuals from infections. The higher up CBC report shows that the patient'due south full white prison cell count is 1.5, which is lower than the normal range of four.0-10.v. The depression white cell count increases the adventure of infection.
Differential: This portion of the CBC shows the counts for the five chief kinds of white cells, either as percentages (the outset 5 counts), or every bit the accented number of cells (the second five counts).
Absolute neutrophil count: Neutrophils are the chief white blood prison cell for fighting or preventing bacterial or fungal infections. In the CBC study, neutrophils may exist referred to as polymorphonuclear cells (polys) or neutrophils. The absolute neutrophil count (ANC) is a measure out of the full number of neutrophils present in the blood. When the ANC is less than 1,000, the risk of infection increases. The ANC can be calculated by multiplying the total WBC by the per centum of polymorphonuclear cells. For example, this patient's ANC is .34 = (WBC) i.5 x 23%.
Ruby-red blood cells: Reddish blood cells carry oxygen from the lungs to the residue of the body. The above CBC report indicates that the patient has a crimson cell count of three.five, which is lower than the normal range of four.lxx-6.10, and therefore, shown in the flag column.
Hemoglobin (Hb or Hgb): Hemoglobin is the office of the red prison cell that carries the oxygen. The above CBC report indicates that the patient's Hb count is 10.8, which is below the normal range of xiv.0-xviii.0. The hematocrit (HCT), another style of measuring the corporeality of Hb, is too depression. This ways that the patient has mild anemia and may be starting to discover symptoms.
Scroll to Continue
These iii ranges will vary depending on historic period and gender. For women, they volition be lower than those shown here. For example, the Hb reference interval for a woman is 12.0-xvi.0.
Platelets: Platelets are the cells that form blood clots that stop haemorrhage. The to a higher place CBC report indicates that the platelet count for this patient is low.
Can Chemotherapy Induced Thrombocytopenia exist Prevented
Chemotherapy-induced thrombocytopenia occurs because the chemotherapy drugs have destroyed many of the normal rapidly dividing cells in the bone marrow responsible for platelet production. Naturally occurring substances called cytokines exist in the body to regulate certain critical functions at the cellular level. One group of cytokines is commonly referred to as claret cell growth factors. Blood prison cell growth factors are responsible for stimulating the cells in the bone marrow to produce more blood cells.
A claret cell growth factor that is approved by the U.S. Food and Drug Administration (FDA) for the prevention of chemotherapy-induced thrombocytopenia is Neumega® (oprelvekin). Neumega helps the os marrow create more platelets and has been demonstrated in clinical studies to prevent thrombocytopenia and decrease the demand for platelet transfusions in patients at high chance for developing thrombocytopenia. The most common side event observed with Neumega is fluid retentivity or edema. This symptom persists while Neumega is being used and is reversible within a few days of discontinuation of Neumega.
How is Chemotherapy Induced Thrombocytopenia Treated
The nearly common mode to treat thrombocytopenia is with platelet transfusions. Transfusions merely temporarily correct thrombocytopenia and are associated with complications.
Platelet Transfusion: The goal of a platelet transfusion is to prevent or stop bleeding. Traditionally, the assessment of a patient for a platelet transfusion was based on a clinical "trigger" value, which is a laboratory value beneath which a transfusion was automatically prescribed. However, transfusions are associated with complications. It is important to carefully evaluate all options when considering a platelet transfusion, every bit the benefits should outweigh the take chances or complications of transfusion.
Although improvements accept lowered the take a chance of transfusion-transmitted complications, the simply way to effectively eliminate the risk is to avoid exposure to allogeneic blood. Despite the risks, platelet transfusions are mutual treatments for thrombocytopenia associated with cancer and chemotherapy.
Complications of Platelet Transfusion: Patients receiving platelet transfusions are at risk for several reactions that range from balmy allergic reactions to life-threatening anaphylaxis. Febrile reactions are the most common, occurring in 1 in every 100 transfusions, but most are not a significant clinical problem. Clinically, the well-nigh significant complications are the immunomodulatory effects of alloimmunization, immunosuppression and graft-versus-host illness (GVHD), all of which are rare.
Infectious Complications: Patients receiving platelet transfusions are at adventure for bacterial, parasitic and viral infections. Bacterial infections are estimated to occur in 1 of every 2,500 transfusions and viral infections occur in approximately ane in every 3,000. Fear of infection with the human immunodeficiency virus (HIV) has caused the well-nigh business organization, although the chance per transfusion is relatively low (1 in 225,000 transfusions). All blood components are tested for HIV antibodies; however, at that place is a catamenia of time after HIV exposure earlier antibodies can exist detected in the blood. To accost this event, intense donor screening is being used and more sensitive assays are being developed.
Patients receiving an allogeneic transfusion are at greater risk for lethal infection for the hepatitis viruses than from HIV. Information technology is estimated that hepatitis results from approximately i in every 3,000 transfusions.
Strategies to Improve Treatment or Prevention of Chemotherapy Induced Thrombocytopenia
The reduction in the frequency and severity of thrombocytopenia and its associated complications has resulted from scientists developing a amend understanding of the basic biology of bone marrow claret cell production and from participation in clinical studies designed to evaluate strategies directed at reducing thrombocytopenia and its complications. Currently, in that location are several strategies aimed at improving the prevention and management of thrombocytopenia.
New blood cell growth factors: Several new blood prison cell growth factors are being developed and evaluated in clinical studies for the purpose of improving chemotherapy-induced thrombocytopenia.
AMG 531 is an investigative amanuensis that stimulates the body to produce platelets and thus reduce or opposite thrombocytopenia. Researchers associated with the AMG 531 in Myelodysplastic Syndrome Study Group conducted a clinical trial to evaluate AMG 531 among patients with myelodysplastic syndrome (MDS) who had thrombocytopenia.[ane] This trial included 28 patients, nine of whom had to receive platelet transfusions to reduce thrombocytopenia.
- 61% of patients had an elevated level of platelets following therapy with AMG 531.
- Nearly one-half of the patients maintained elevated levels of platelets for eight or more weeks.
The researchers concluded that AMG 531 appears to provide promising action among patients with MDS who have thrombocytopenia. Ultimately, AMG 531 may significantly reduce the demand for platelet transfusions and prevent bleeding in this group of patients. Time to come clinical trials are planned to further evaluate AMG 531 in this setting.
Peripheral blood stem cells: Stem cells responsible for the production of platelets tin exist collected in large quantities from the peripheral blood. Delivery of peripheral blood stem cells following very loftier doses of chemotherapy has been demonstrated to result in more rapid platelet recovery than with stem cells collected from bone marrow. Many doctors accept begun evaluating the apply of peripheral blood stem cells to support multiple cycles of dose intensive chemotherapy alone or in combination with Neumega® or other blood cell growth factors for the purpose of reducing the frequency and severity of thrombocytopenia and its complications.
Reference:
[1] Kantarjian HM, Giles FJ, Fenauz P, et al. Evaluating safety and efficacy of AMG 531 for the handling of thrombocytopenic patients with myelodysplastic syndrome (MDS): Preliminary results of a Phase 1-two study. Proceedings from the 2007 almanac meeting of the American Social club of Clinical Oncology. Abstruse 7032.
- Managing Side Effects of Cancer Treatment
- For news on cancer updates, research and education subscribe to Cancer Connect's newsletters here.
- Connect with other patients and caregivers for data and support hither.
How Long Does It Take For Platelets To Increase After Chemo,
Source: https://news.cancerconnect.com/treatment-care/side-effects-of-cancer-treatment-thrombocytopenia-low-platelet-counts
Posted by: baileywarailut.blogspot.com


0 Response to "How Long Does It Take For Platelets To Increase After Chemo"
Post a Comment